Compressed air quality standard verification in the international medical field
Compressed air and gas are vital to the operation of many medical facilities, and are usually used for breathing, sedation, and the operation of medical devices. Medical facilities must rely on these facilities to save lives and treat. The quality of the air and gas produced by the facility’s compressed air system is critical to its effectiveness in promoting positive patient prognosis.
Compressed air/gas pollution, whether it comes from ambient air, the air compressor itself, or the pipeline system, is the responsibility of medical facilities, which may threaten the health and safety of patients, and ultimately lead to medical facilities causing litigation losses in medical accidents.
In 1996, trichloroethylene (a solvent commonly used to clean pipelines and gas tanks) contaminated its bulk oxygen tanks [1], resulting in at least 4 deaths and 70 injuries. Hospital staff noticed an odor soon after the tank was replaced [1], which is an obvious sign of pollution that should not be ignored, and it happens to be the National Fire Protection Association (NFPA) health care facility regulations [2] Part of the air/gas standard
Understanding NFPA 99
Regulatory agencies, including the Centers for Medicare and Medicaid Services (CMS), Joint Commission (TJC), and Local Authorities with Jurisdiction (AHJ), require medical facilities to ensure that their compressed air and gas systems comply with NFPA 99.
NFPA 99 lists odor, water, carbon monoxide, carbon dioxide, gaseous hydrocarbons, halogenated hydrocarbons, oil, and particulates as the main pollutants to monitor and set the concentration and purity requirements of medical gases shown in Table 1.
According to Kyle Jussel, an experienced and certified medical gas system verifier and Chairman of the Medical Gas Professional Medical Organization (MGPHO), “NFPA 99 requires that as a verifier, we conduct initial tests (for these contaminants) at the source and at each point of use. The facility is also required to show that each accessible medical gas export/import has been tested and inspected based on its own risk assessment, taking into account the equipment manufacturer’s recommendations, and then usually tested and inspected annually."
Note that NFPA 99 does not include specific standards for live particles, such as bacteria, mold and yeast. However, for medical facilities, it is important to verify whether the compressed air and gas have potential microbial contamination.
Understand regulated pollutants
Before delving into the negative effects of pollution, it is important to understand how pollution occurs. According to Jussel, one of the main sources of contamination that we usually see when verifying medical gas systems includes copper particles, which are usually caused by installers who did not perform adequate cleaning during the initial test. We occasionally see signs of blockages in combustion pipes that were never removed before installation. According to NFPA 99, it is easy to find during the odor test required by the verifier. However, contamination is not just a problem observed during installation and verification. Jussel explained that; once the system was properly installed, verified, and put into use for patients, we found problems with high levels of carbon monoxide, carbon dioxide, and humidity/dew point. All of these may be caused by maintenance-related issues or poor intake air quality.

Understanding the pollutants specified by NFPA 99 and their potential adverse effects is not only essential to comply with NFPA 99 air/gas standards, but also to ensure the quality of medical gases used in medical facilities. Examples are shown in Table 2.
As shown in Table 2, it needs to be reiterated that contamination or deviation of gas purity may lead to life-threatening patients. NFPA 99 only provides for newly installed, repaired or modified compressed air and gas systems and extensive air/gas verification based on the recommendations of the air compressor manufacturer [2]. Compressed air and gas systems that do not meet these standards, such as previously verified and old systems, can be exempted from additional verification under NFPA 99. However, NFPA 99 does require air quality monitors, although the monitoring may not include or individually identify all pollutants tested during verification, such as halogenated hydrocarbons such as trichloroethylene. Therefore, it is beneficial to continuously monitor and test the compressed air and gas systems of medical institutions to protect patient safety, achieve high compressed air system efficiency to save money, and provide evidence in legal affairs.
Compressed air and gas verification test
To ensure compliance with NFPA 99, medical facilities must complete verification tests for pipeline cleaning, pipeline particulates, pipeline purity, medical gas purity, and medical gas concentration (see Table 2).
NFPA 99 requires testing/analysis by a party other than the installer [2]. When the system is not installed by internal personnel, it can be tested by internal American Society of Safety Engineers (ASSE) 6030 qualified employees. ASSE 6030 qualified employees can use portable analyzers/monitors or work with third-party laboratories to complete verification tests in accordance with NFPA 99. This enables medical institutions to save money and proactively minimize risks to patients and institutions.
Portable analyzers and third-party laboratory testing methods have their own advantages. ``For example, portable analyzers can provide faster results and real-time performance. However, due to more complex technology, instruments and data analysis, laboratory tests usually have higher accuracy and quality. Therefore, testing laboratories can sometimes provide clues about the source of pollution by describing/identifying particles, hydrocarbons, oil, etc. If a laboratory is used for analysis, it is in the best interest of medical institutions to use only accredited testing laboratories (such as Trace Analytics, LLC), because it can ensure that analysts, test equipment, methods, quality assurance and test data meet or exceed international standards Recognized standards (such as ISO 17025 for testing laboratories). Jussel said that by sending air samples to a third-party laboratory for analysis, we can give our customers peace of mind because we know that the air quality they provide to patients has undergone additional tests.
Jussel went on to explain that; not only was the medical air system tested at startup/verification, but it was also continuously monitored by the air quality monitor required by NFPA 99. The results can also be compared with the third-party laboratory analysis we provide every year.
In addition to providing objective guarantees for medical facilities, in the long run, third-party laboratory testing may be cheaper. If maintained by the medical institution itself, portable analyzers may be overlooked because they are expensive, require calibration and frequent maintenance. In this regard, medical facilities should determine their verification and continuous testing requirements based on the facility-specific risk assessment.
Use proper air handling
The use of proper air treatment is essential to meet the air/gas quality requirements of NFPA 99.
In order to prevent water pollution, it is common to place desiccants and install dryers in medical equipment to remove water from compressed air/gas, because NFPA 99 requires the maximum dew point of the dryer outlet air to be less than 32;F under 50-55 psi2 conditions. Although freeze dryers are effective in many applications, they generally cannot provide air below 35F dew point, especially under low flow conditions common in hospitals, because centrifugal separators cannot effectively remove condensate. The dryer system is usually redundant, and NFPA 99 requires a duplex system to prevent water pollution in the event of a failure. The desiccant dryer can release particles into the compressed air system, because the desiccant is constantly moving/friction as the air flows through it will generate desiccant dust. This explains how the compressed air system and air treatment itself produce pollutants, so these pollutants must be constantly monitored and controlled. A series of filters can be used to remove particles from ambient air or the air compressor itself. It should be noted that point-of-use filters are essential to ensure that compressed air/gas is free of particles during use. Condensate oil is another pollutant analyzed by the NFPA 99 verification test. When an oil lubrication system is used, it may come from an air compressor or ambient air. In order to remove condensate oil, a coalescing filter can be used. For gaseous pollutants, such as volatile hydrocarbons and carbon dioxide, activated carbon filters/towers and catalytic converters can be used respectively.
Air treatment can not only remove pollution, but also make the compressed air system work more efficiently, saving money by extending the service life of the air compressor and making the system work faster. Adopting air handling and performing air compressor maintenance, combined with compressed air/gas testing, enables medical facilities to ensure this utility and the quality of treatment.
Test frequency and trend analysis
NFPA 99 requires verification tests for new, improved or repaired compressed air systems, and follow-up tests according to the manufacturer’s recommendations, usually once a year. However, this testing frequency may not be sufficient to ensure the quality of compressed air/gas throughout the year. Some facilities may choose to conduct a test every quarter because seasonal changes can change the quality of compressed air/gas. For example, high concentrations of water are more common in summer than in winter [3]. Other facilities can be tested before and after compressor repair to ensure that the repair will not cause pollution.
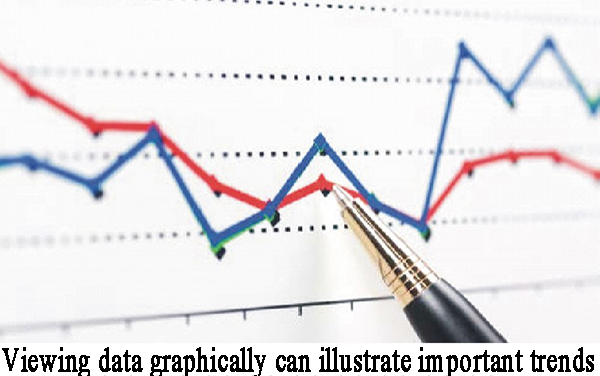
It is important to understand that the test only provides data for the compressed air system at the time of sampling. To best optimize testing to ensure compressed air/gas quality, trend analysis can be used. Trend analysis can use the air quality monitoring data obtained from the monitors required by NFPA 99, combined with third-party laboratory test data, to provide detailed air quality changes over time. The compressed air system is dynamic; seasonal changes, system wear and other factors will affect the air/gas quality. Over time, collecting enough data to account for seasonal and maintenance changes and allow medical institutions to establish baseline quality levels of pollutants. The facility can best determine the maintenance/cleaning plan of the air compressor, potentially saving the facility time and money. In addition to establishing a baseline, medical institutions can also set action and alarm levels, which allow the institution to predict contamination issues before issuing surveillance alarms or threatening patient safety.
Ensure patient safety through testing and monitoring
NFPA 99 "Medical Facilities Specification" is an important standard to ensure the quality and safety of compressed air and gas used in medical facilities. Deviations in air purity and pollution may endanger the safety of patients. In order to comply with NFPA 99 and protect patients, medical facilities should adopt air treatment and conduct routine compressed air/gas testing and monitoring.
references
[1] Moss, E. and Evans, F. Hospital Deaths. Anesthesia Patient Safety Foundation. Retrieved July 27, 2019 from https://www.apsf.org/article/ hospital-deaths/
[2] NFPA 99 Healthcare Facilities Code (2018)
[3] Water Vapor. Trace Analytics, LLC. Retrieved August 2, 2019 from https:// www.airchecklab. com/aircheck-academy/breathing-air/sources-ofcontamination/water-vapor/
[4] Mould, damp and the lungs. European Respiratory Society. Retrieved July 28, 2019 from https:// www.ncbi.nlm.nih.gov/pmc/articles/PMC5709805/
[5] Allen, E. E. (2018). Medical Gas System Safety. The Doctor's Company. Retrieved July 20, 2019 from https://www.thedoctors.com/articles/ medicalgas-system-safety/
[6] Moss, E. Medical Air. Anesthesia Patient Safety Foundation. Retrieved July 21, 2019 from https://www.apsf.org/article/medical-air/
[7] Carbon Monoxide Poisoning. Centers for Disease Control and Prevention. Retrieve July 19, 2019 from https:// ephtracking.cdc.gov/showCoRisk.action
[8] Pietro, M. (2018). Humidity levels and COPD. Medical News Today. Retrieved July 21, 2019 from https://www.medicalnewstoday.com/articles/323657. php
[9] Carbon Dioxide OSH Answers Fact Sheets. (2019). Canadian Centre for Occupational Health and Safety. Retrieved August 1, 2019 from https://www. ccohs.ca/oshanswers/chemicals/chem_profiles/carbon_dioxide.html
[10] Toluene OSH Answers Fact Sheets. (2019). Canadian Centre for Occupational Health and Safety. Retrieved August 1, 2019 from https://www.ccohs.ca/ oshanswers/chemicals/chem_profiles/toluene.html
[11] Trichloroethylene OSH Answers Fact Sheets. (2019). Canadian Centre for Occupational Health and Safety. Retrieved August 1, 2019 from https://www. ccohs.ca/oshanswers/chemicals/chem_profiles/trichloroethylene.html
[12] Brown, K. W. and Armstrong, T. J. (2019). Hydrocarbon Inhalation. StatPearls. Retrieved July 21, 2019 from https://www.ncbi.nlm.nih.gov/books/ NBK470289/
[13] Breathing Air Quality, Sampling and Testing. Environmental Health Laboratory, department of Environmental and Occupational Health Sciences, School of Public Health, University of Washington. Retrieved July 28, 2019 from https://deohs.washington.edu/ sites/default/files/images-envhlth/topic/ BreathingAirQualitySamplingandTesting_Technical.pdf
[14] Francis, J. Breathing Gas Contamination. Divers Alert Network. Retrieved August 1, 2019 from https://www.diversalertnetwork.org/health/PSAGasContamination/index.html
[15] Particle Pollution and Your Health. U.S. Environmental Protection Agency. Retrieved July 28, 2019 from https://nepis.epa.gov/Exe/ZyPDF. cgi?Dockey=P1001EX6.txt
[16] Health and Environmental Effects of Particulate Matter (PM). U.S. Environmental Protection Agency. Retrieved July 27, 2019 from https://www. epa.gov/pm -pollution/health-and-environmental-effects-particulate-matterpm
Moss, E. Medical Gas Contamination An Unrecognized Patient Danger. Anesthesia Patient Safety Foundation. Retrieved August 2, 2019 from https://www.apsf.org/article/ medical-gas-contamination-an-unrecognizedpatient-danger/


